- Rectal bleeding
- Rectal pain
- Urgency in your bowel movements
Dr.Bhavik Rana(Consultant)|Vapi & Valsad
+91-97242 47109
What is Ulcerative Colitis?
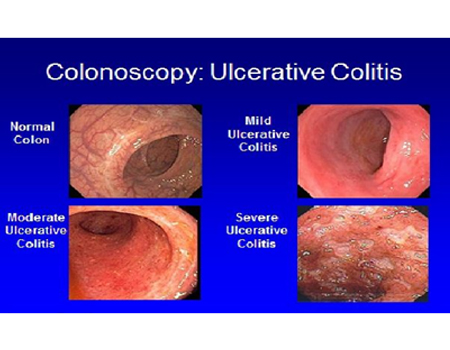
Ulcerative colitis is a chronic disease of the large intestine, in which the lining of the colon becomes inflamed and develops tiny open sores, or ulcers. This condition is the result of your immune system’s overactive response.
We can help you with information and resources to get you feeling better physically and emotionally.
Those ulcers produce pus and mucous, which cause abdominal pain and the need to frequently empty your colon.
What is Ulcerative Colitis?
Ulcerative colitis is the result of several factors that are not yet well understood. Abnormal immune response, genetics, microbiome, and environmental factors all contribute to ulcerative colitis.
Research suggests that ulcerative colitis could be triggered by an interaction between a virus or bacterial infection in the colon and the body’s immune response.
Typically, the cells and proteins that make up your immune system protect you from infection.
A normal immune response would cause temporary inflammation to combat an illness or infection. The inflammation would then go away once you are healthy and free of the illness.
In ulcerative colitis patients, the inflammation persists long after the immune system should have finished its job. The body continues to send white blood cells into the lining of the intestines, where they produce chronic inflammation and ulcers.
Ulcerative colitis can occur at any age, though most people are diagnosed in their mid-30s.
Men and women are equally likely to be affected, but older men are more likely to be diagnosed than older women.
The risk of developing ulcerative colitis is between 1.6 percent and 30 percent if you have a first-degree relative with the disease.1-3
It is not possible to confidently predict which, if any, family members will develop ulcerative colitis, even though there is an increased risk of IBD based on family history.
Ulcerative colitis can affect people of any racial or ethnic group.
1. Ulcerative Proctitis
In ulcerative proctitis, bowel inflammation is limited to the rectum. This condition typically affects less than six inches of the rectum, and it is not associated with an increased risk of cancer.
Symptoms may include:
2. Left-Sided Colitis
In this form of ulcerative colitis, continuous inflammation begins at the rectum and extends as far into the colon as the splenic flexure, which is a bend in the colon near the spleen. Left-sided colitis also includes proctosigmoiditis, which affects rectum and the lower segment of colon located right above the rectum known as the sigmoid colon.
Symptoms may include:
3. Extensive Colitis
This type of ulcerative colitis affects the entire colon. Continuous inflammation begins at the rectum and extends beyond the splenic flexure.
Symptoms may include:
There are several symptoms of ulcerative colitis that can affect your general health and your quality of life.
The primary goal in treating ulcerative colitis is to help patients regulate their immune system better. While there is no known cure for ulcerative colitis and flare ups may recur, a combination of treatment options can help you stay in control of your disease and lead a full and rewarding life.
Treatment for ulcerative colitis is multifaceted and includes the use of medication, alterations in diet and nutrition, and sometimes surgical procedures to repair or remove affected portions of your GI tract.
Medication for ulcerative colitis can suppress the inflammation of the colon and allow for tissues to heal. Symptoms including diarrhea, bleeding, and abdominal pain can also be reduced and controlled with effective medication.
In addition to controlling and suppressing symptoms (inducing remission), medication can also be used to decrease the frequency of symptom flare ups (maintaining remission). With proper treatment over time, periods of remission can be extended and periods of symptom flare ups can be reduced. Several types of medication are being used to treat ulcerative colitis today.
In some circumstances, a health care provider may recommend adding an additional therapy that will work in combination with the initial therapy to increase its effectiveness. For example, combination therapy could include the addition of a biologic to an immunomodulator. As with all therapy, there are risks and benefits of combination therapy. Combining therapies can increase the effectiveness of IBD treatment, but there may also be an increased risk of additional side effects and toxicity. Your healthcare provider will identify the treatment option that is most effective for your individual health care needs.
While ulcerative colitis is not caused by the foods you eat, you may find that once you have the disease, particular foods can aggravate the symptoms. It’s important to maintain a healthy and soothing diet that helps reduce your symptoms, replace lost nutrients, and promote healing.
For people diagnosed with ulcerative colitis, it is essential to maintain good nutrition because the disease often reduces your appetite while increases your body’s energy needs. Additionally, common symptoms like diarrhea can reduce your body’s ability to absorb protein, fat, carbohydrates, as well as water, vitamins, and minerals.
Many people with ulcerative colitis find that soft, bland foods cause less discomfort than spicy or high-fiber foods. While your diet can remain flexible and should include a variety of foods from all food groups, your doctor will likely recommend restricting your intake of dairy foods if you are found to be lactose-intolerant.