- Most commonly occurs at the end of the small intestine
- May appear in patches
- May extend through entire thickness of bowel wall
- About 67% of people in remission will have at least 1 relapse over the next 5 years
Dr.Bhavik Rana(Consultant)|Vapi & Valsad
+91-97242 47109
Crohn’s disease is a chronic inflammatory bowel disease (IBD) characterized by inflammation of the digestive, or gastrointestinal (GI) tract. In fact, Crohn’s can affect any part of the GI tract, from the mouth to the anus, but it is more commonly found at the end of the small intestine (the ileum)
where it joins the beginning of the large intestine (or colon). It can also affect:Eyes ,Skin, Joint
Both Crohn’s disease and ulcerative colitis (UC) are inflammatory bowel diseases (IBDs), but there are some key differences.
Inflammation may develop anywhere in the GI tract from the mouth to the anus
Symptoms may include:
Ulcerative colitis
Limited to the large intestine (colon and rectum)
Symptoms may include:
Crohn’s disease symptoms range from mild to severe. They may vary over time and from person to person, depending on what part of the gastrointestinal (GI) tract is inflamed. And because symptoms vary from person to person, the way to gauge what you consider a flare-up of symptoms is relative to what is “normal” for you.
Common Crohn’s disease symptoms include:
Crohn’s can affect the entire GI tract — from the mouth to the anus — and can be progressive, so over time, your symptoms could get worse. That's why it's important that you have an open and honest conversation about your symptoms, since your doctor will use that information to help determine what treatment plan is best for you.
It might be helpful to refer to the chart below to help you understand the differences between mild, moderate and severe symptoms, since your doctor may use similar measures.
Mild to Moderate
You may have symptoms such as:
No signs of:
Moderate to Severe
You may have symptoms such as:
Significant anemia (a few of these symptoms may include fatigue, shortness of breath, dizziness and headache)
Very Severe
Persistent symptoms despite appropriate treatment for moderate to severe Crohn’s, and you may also experience:
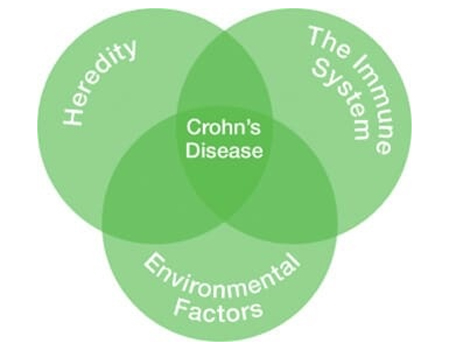
While its exact causes are unknown, what is known is that Crohn’s disease is a chronic, or ongoing, inflammatory bowel disease (IBD) that primarily affects the digestive or gastrointestinal (GI) tract. Crohn’s inflammation can develop anywhere from the mouth to the anus, and symptoms may vary depending on what part of the GI tract is inflamed. You may experience symptoms that occur outside the GI tract, affecting the eyes, skin and joints. Crohn’s is not contagious, nor is it caused by something you may have done or eaten.
The immune system is a complex network of cells that interact with each other to defend the body against foreign invaders Circulating white blood cells patrol for foreign invaders, such as bacteria or viruses, “non-self” cells, which are considered dangerous
While Crohn’s disease most often starts between the ages of 15 and 35, it can affect people of any age.
Crohn’s disease affects men and women equally, and it appears to be more common in people in developed countries and among the Ashkenazi Jewish population.